PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1846318

PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1846318
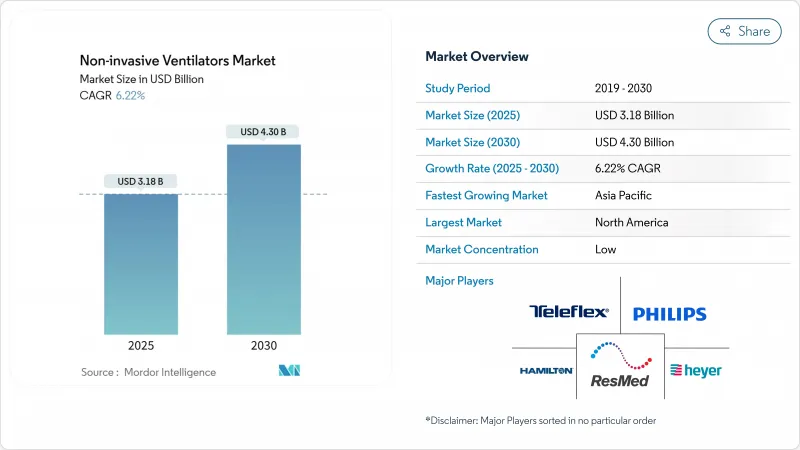
Non-invasive Ventilators - Market Share Analysis, Industry Trends & Statistics, Growth Forecasts (2025 - 2030)
The non-invasive ventilator market stood at USD 3.18 billion in 2025 and is forecast to reach USD 4.30 billion by 2030, advancing at a 6.22% CAGR.
Demand is shifting from pandemic-driven surges to secular growth anchored in chronic respiratory disease management, geriatric care requirements and rising home-based therapy adoption. Artificial-intelligence algorithms that fine-tune pressure delivery, together with simplified negative-pressure concepts for resource-limited settings, are broadening the clinical footprint of the non-invasive ventilator market. Device makers focus on comfort-oriented interfaces, noise reduction and cloud connectivity to keep patients on therapy, while payers in the United States and selected European Union countries expand reimbursement to ease budget constraints. Asia-Pacific healthcare build-outs, semiconductor supply-chain stabilization and FDA fast-track clearances for portable platforms support a resilient outlook for the non-invasive ventilator market beyond traditional hospital walls.
Global Non-invasive Ventilators Market Trends and Insights
Surging Prevalence of COPD & Asthma Cases
More than 390 million people live with COPD and 262 million with asthma worldwide, generating steady demand for advanced ventilation support. Meta-analyses show that long-term non-invasive ventilation reduces mortality in obstructive sleep apnea and hypercapnic COPD cohorts. The 2025 GOLD report adds cardiovascular risk control and climate-related exacerbation management to treatment pathways, favoring intelligent ventilation that adapts to fluctuating physiology. Average Volume Assured Pressure Support paired with transcutaneous CO2 monitoring lowers 48-hour reintubation risk and shortens stays for acute-on-chronic COPD cases. Real-time analytics platforms further personalize therapy and cut unplanned admissions by predicting decompensation events.
Increasing ICU Admissions Among Geriatrics
Adults over 65 account for a growing portion of intensive-care occupancy, often presenting with respiratory failure and multiple comorbidities. Non-invasive ventilation reduces inspiratory effort and improves tidal volumes in elderly patients compared with high-flow nasal oxygen. Device protocols now incorporate lower trigger thresholds and synchrony features to match diminished muscle strength, lowering extubation failure odds. Health systems expand ICU beds yet prefer NIV to avoid invasive airway complications and to shorten length of stay, protecting budgets while raising quality scores.
Ventilator-Associated Pneumonia Risk
VAP incidence ranges from 9.2% to 30% in mechanically ventilated cohorts, adding roughly USD 544,467 per case to hospital bills versus non-VAP patients. Diagnostic variability complicates prevention, prompting global infection societies to standardize bundles that combine head-of-bed elevation, circuit hygiene and early mobilization. While NIV avoids intubation, mask leaks and secretion buildup can still seed infection, requiring design tweaks such as automatic secretion drainage and antimicrobial surfaces. Education campaigns in low- and middle-income countries show that bundle adherence cuts VAP rates by up to 35%, protecting fragile budgets.
Other drivers and restraints analyzed in the detailed report include:
- Shift Toward Home-Based NIV Therapy
- Reimbursement Expansion for Home NIV
- High Device & Maintenance Cost
For complete list of drivers and restraints, kindly check the Table Of Contents.
Segment Analysis
The non-invasive ventilator market size for positive-pressure devices stood at USD 1.98 billion in 2025, corresponding to a 62.36% revenue share that reflects their entrenched role in acute and chronic care settings. Continuous Positive Airway Pressure and Bilevel PAP remain gold standards for obstructive sleep apnea and COPD exacerbations, benefiting from auto-adjusting algorithms that calibrate pressure in five-millisecond cycles. Manufacturers add humidification controls and noise-attenuation chambers to lift adherence above 80% during the first 90 days of therapy. Cloud-native dashboards push ventilatory parameters to clinicians, allowing remote titration that reduces follow-up visits. Patient-facing mobile apps gamify nightly use and flag mask-fit issues in real time.
Negative-pressure ventilators are experiencing a technical renaissance, recording the fastest 7.15% CAGR through 2030. Modern shells use lightweight composites and compact vacuum pumps, enabling patients to sit upright, converse and ingest food without therapy interruption. Clinical studies in acute respiratory distress syndrome report 15% higher PaO2/FiO2 ratios compared with positive-pressure modes, suggesting lung-protective advantages. Philanthropic consortia fund open-source designs aimed at district hospitals in low-resource geographies, and regulatory agencies have published fast-track guidelines to validate essential safety features.
The Non-Invasive Ventilator Market Report is Segmented by Product (Non-Invasive Positive-Pressure Ventilator, Non-Invasive Negative-Pressure Ventilator), Application (COPD & Asthma, and More), End User (Hospitals & Clinics, Ambulatory Surgical Centers, Homecare Settings), and Geography (North America, Europe, Asia-Pacific, Middle East & Africa, South America). The Market Forecasts are Provided in Terms of Value (USD).
Geography Analysis
North America commanded 43.45% of non-invasive ventilator market revenue in 2024 on the back of high disease prevalence, sophisticated reimbursement and rapid device approvals. The FDA granted 510(k) clearance to the Servo-air portable ventilator in June 2024, adding choice for outpatient programs. CMS's national coverage analysis for home NIV therapy is expected to widen beneficiary access in late 2025, stimulating supplier investment in cloud ecosystems. Data-integration mandates encourage interoperability between ventilators, electronic health records and payer portals, creating a virtuous cycle of evidence generation and reimbursement reinforcement.
Asia-Pacific records the fastest 8.14% CAGR through 2030. Healthcare expenditure in China surpassed CNY 8.5 trillion in 2022 and is projected to hit CNY 20.5 trillion by 2030, enabling tertiary-care network upgrades . Governments introduce pilot schemes for negative-pressure ventilation kits in rural clinics to address acute pneumonia outbreaks without relying on scarce intensive-care beds. Local assembly lines shorten lead times and insulate procurement from currency volatility. Regional academic partnerships generate data on NIV efficacy in tuberculosis-coexistent COPD, guiding tailored protocols.
Europe stabilizes growth at mid-single digits, supported by universal health systems and stringent safety standards. The European Respiratory Society's latest guideline endorses early application of NIV in postoperative respiratory failure, feeding procurement pipelines for high-flow capable machines. ESG initiatives push suppliers to design recyclable circuits and to measure carbon footprints across the ventilator life cycle.
Middle East & Africa and South America contribute modest base-effect expansion. Oil-exporting economies channel surplus revenue into critical-care capacity, while public-private partnerships in Brazil fund tele-ventilation projects that connect secondary hospitals with urban pulmonology hubs. Development banks back equipment-leasing pools to sidestep high import tariffs, further democratizing access.
- Resmed
- Koninklijke Philips
- Fisher & Paykel Healthcare
- Hamilton Medical
- Teleflex
- Medtronic
- GE Healthcare
- Dragerwerk
- Vyaire Medical
- Nihon Kohden Corp.
- Smiths Group
- Getinge
- Airon
- Air Liquide
- Ventec Life Systems
- Phoenix Medical Systems
- Heyer Medical
- Zoll Medical Corp.
Additional Benefits:
- The market estimate (ME) sheet in Excel format
- 3 months of analyst support
TABLE OF CONTENTS
1 Introduction
- 1.1 Study Assumptions & Market Definition
- 1.2 Scope of the Study
2 Research Methodology
3 Executive Summary
4 Market Landscape
- 4.1 Market Overview
- 4.2 Market Drivers
- 4.2.1 Surging Prevalence Of COPD & Asthma Cases
- 4.2.2 Increasing Icu Admissions Among Geriatrics
- 4.2.3 Shift Toward Home-Based NIV Therapy
- 4.2.4 Reimbursement Expansion For Home NIV
- 4.2.5 AI-Driven Closed-Loop Niv Modes Gain Traction
- 4.2.6 Rise Of Low-Cost Negative-Pressure NIV Devices For Lmics
- 4.3 Market Restraints
- 4.3.1 Ventilator-Associated Pneumonia (Vap) Risk
- 4.3.2 High Device & Maintenance Cost
- 4.3.3 Skill Gap In Handling Advanced NIV Modes
- 4.3.4 Supply-Chain Fragility For Critical Components
- 4.4 Value / Supply-Chain Analysis
- 4.5 Regulatory Landscape
- 4.6 Technological Outlook
- 4.7 Porter's Five Forces Analysis
- 4.7.1 Threat of New Entrants
- 4.7.2 Bargaining Power of Buyers
- 4.7.3 Bargaining Power of Suppliers
- 4.7.4 Threat of Substitutes
- 4.7.5 Competitive Rivalry
5 Market Size & Growth Forecasts (Value)
- 5.1 By Product
- 5.1.1 Non-invasive Positive-pressure Ventilator (PPV)
- 5.1.1.1 Bi-level Positive Airway Pressure (BiPAP)
- 5.1.1.2 Constant Positive Airway Pressure (CPAP)
- 5.1.1.3 Autotitrating Positive Airway Pressure (APAP)
- 5.1.2 Non-invasive Negative-pressure Ventilator (NPV)
- 5.1.1 Non-invasive Positive-pressure Ventilator (PPV)
- 5.2 By Application
- 5.2.1 COPD & Asthma
- 5.2.2 Respiratory Distress Syndrome
- 5.2.3 Others
- 5.3 By End User
- 5.3.1 Hospitals & Clinics
- 5.3.2 Ambulatory Surgical Centers
- 5.3.3 Homecare Settings
- 5.4 By Geography
- 5.4.1 North America
- 5.4.1.1 United States
- 5.4.1.2 Canada
- 5.4.1.3 Mexico
- 5.4.2 Europe
- 5.4.2.1 Germany
- 5.4.2.2 United Kingdom
- 5.4.2.3 France
- 5.4.2.4 Italy
- 5.4.2.5 Spain
- 5.4.2.6 Rest of Europe
- 5.4.3 Asia-Pacific
- 5.4.3.1 China
- 5.4.3.2 Japan
- 5.4.3.3 India
- 5.4.3.4 Australia
- 5.4.3.5 South Korea
- 5.4.3.6 Rest of Asia-Pacific
- 5.4.4 Middle East & Africa
- 5.4.4.1 GCC
- 5.4.4.2 South Africa
- 5.4.4.3 Rest of Middle East & Africa
- 5.4.5 South America
- 5.4.5.1 Brazil
- 5.4.5.2 Argentina
- 5.4.5.3 Rest of South America
- 5.4.1 North America
6 Competitive Landscape
- 6.1 Market Concentration
- 6.2 Market Share Analysis
- 6.3 Company Profiles {(includes Global level Overview, Market level overview, Core Segments, Financials as available, Strategic Information, Market Rank/Share, Products & Services, Recent Developments)}
- 6.3.1 ResMed Inc.
- 6.3.2 Koninklijke Philips N.V.
- 6.3.3 Fisher & Paykel Healthcare
- 6.3.4 Hamilton Medical AG
- 6.3.5 Teleflex Incorporated
- 6.3.6 Medtronic plc
- 6.3.7 GE Healthcare
- 6.3.8 Draegerwerk AG & Co. KGaA
- 6.3.9 Vyaire Medical
- 6.3.10 Nihon Kohden Corp.
- 6.3.11 Smiths Medical
- 6.3.12 Getinge AB
- 6.3.13 Airon Corporation
- 6.3.14 Air Liquide Medical Systems
- 6.3.15 Ventec Life Systems
- 6.3.16 Phoenix Medical Systems
- 6.3.17 Heyer Medical AG
- 6.3.18 Zoll Medical Corp.
7 Market Opportunities & Future Outlook
- 7.1 White-space & Unmet-need Assessment




