PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1849847

PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1849847
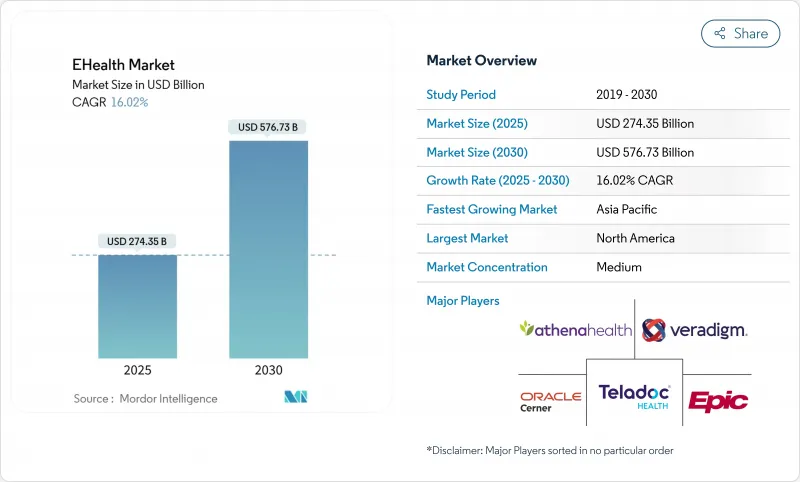
EHealth - Market Share Analysis, Industry Trends & Statistics, Growth Forecasts (2025 - 2030)
The eHealth market reached USD 274.35 billion in 2025 and is forecast to touch USD 576.73 billion by 2030, advancing at a 16.02% CAGR.
This performance stems from rapid gains in connectivity, favorable legislation, and sustained investment in digital-first care pathways that let providers scale services without proportional increases in staff or physical infrastructure. Rising reimbursement for remote monitoring, wider 5G rollouts, and the integration of generative-AI assistants into clinical workflows further expand the addressable patient base, while growing consumer acceptance anchors long-run demand. Health-system mergers now dedicate high capital to IT modernisation, illustrating that digital capabilities have shifted from "nice to have" to "mission critical." Still, data-security incidents and interoperability gaps temper near-term growth ambitions and oblige new spending on cyber-risk mitigation and data-exchange standards.
Global EHealth Market Trends and Insights
Government Incentives For Digital Health Adoption
Financial carrots and regulatory sticks continue to accelerate eHealth market penetration. The HTI-2 rule finalized by the U.S. Department of Health and Human Services penalizes information blocking and forces tighter interoperability, spurring hospital demand for standards-compliant upgrades. Meanwhile, the European Health Data Space secured EUR 810 million to harmonize data exchange across 27 member states, offering vendors a single continental entry point. Australia's 2023-2028 National Digital Health Strategy funds interoperability layers that link federal registries to state systems. Collectively, these programs shorten sales cycles, provide direct subsidy pools, and cement the convening power of governments in setting technical baselines. As compliance dates approach, provider budgets increasingly prioritize certified platforms, creating a pull-through effect for integration consultancies and cybersecurity vendors. The visible policy pipeline increases investor confidence, keeping capital flows robust even in tighter macro conditions.
Growing Prevalence Of Chronic Diseases Demanding Remote Monitoring
Rising incidence of diabetes, hypertension, and COPD shifts care toward continuous at-home oversight and generates recurring device and analytics revenues. Remote patient monitoring adoption reached 81% of U.S. clinicians by 2023 and delivered a 76% drop in 30-day readmissions among high-risk cohorts. Teladoc Health reports a threefold rise in diabetes-member engagement and a 0.4 reduction in A1c through predictive nudges, underscoring clinical validity. Wearable shipments are tracking 55% annual growth as sensors graduate from fitness tracking to FDA-cleared medical functionality. As insurers expand reimbursement codes, device makers bundle AI-powered triage layers that flag deterioration early and escalate only when clinically necessary, trimming utilization costs. High-speed cellular connectivity broadens eligible populations in rural areas, while cloud-native dashboards lower IT overhead for small practices, opening fresh sub-segments of the eHealth market.
Data Security & Privacy Concerns
Cyber incidents reached a record 677 major breaches in 2024, affecting 182.4 million individuals and highlighting persistent attack-surface expansion as devices proliferate. The Change Healthcare ransomware event alone disrupted claims processing nationwide, underscoring the systemic nature of third-party dependencies. Health records command premium dark-web prices because they carry immutable personal identifiers, attracting both cybercriminals and nation-state actors. The HHS cybersecurity strategy now proposes new HIPAA Security Rule standards, while the Health Care Cybersecurity Improvement Act offers funding for small practices to upgrade tools. EU regulators impose heavy fines for GDPR lapses, forcing multinationals to engineer data-minimization workarounds. Ongoing vulnerability management costs and rising cyber-insurance premiums erode margins, causing some providers to defer non-critical digital projects and slowing overall eHealth market adoption.
Other drivers and restraints analyzed in the detailed report include:
- Expansion Of High-Speed Connectivity (5G) Enabling Telehealth
- Integration Of Generative-AI Copilots Into EHR Workflows
- Interoperability Challenges Among Disparate Systems
For complete list of drivers and restraints, kindly check the Table Of Contents.
Segment Analysis
Electronic Health Records generated the largest 39.35% share of the eHealth market in 2024 as regulatory compliance, incentives, and enterprise-grade functionality kept procurement pipelines robust. Cloud-enabled upgrades bundled with analytics and population-health modules have renewed growth, while embedded generative-AI copilots from Epic and Oracle compress documentation time and attract multi-year license renewals. The component's lead positions vendors to cross-sell revenue-cycle and clinical-decision add-ons, sustaining average deal sizes. Telemedicine posted the fastest 20.25% CAGR outlook because post-pandemic consumer familiarity, payment parity laws, and scalable video infrastructure lowered adoption barriers. Amazon's consolidation of Clinic into One Medical signals that platform integration and national brand trust will dictate competitive advantage going forward.
Fast-moving mHealth apps combine smartphone cameras, edge AI, and low-cost sensors to support dermatology, ophthalmology, and mental-health triage, deepening consumer engagement. Clinical Decision Support tools embedded in imaging platforms record higher sensitivity and specificity, reinforcing demand for algorithm training datasets. e-Prescribing exhibits steady expansion under mandatory electronic-controlled-substance regulations, but remains hampered by inconsistent pharmacy system upgrades. Together, diversified component innovation keeps the eHealth market vibrant and spurs ecosystem partnerships.
Cloud platforms supplied 52.53% of 2024 revenue and anchor modernization roadmaps because they eliminate capital-intensive data centers and power automatic patching, essential to cyber-risk management. Microsoft Cloud for Healthcare exemplifies how shared responsibility models and responsible-AI toolchains de-risk adoption while compressing deployment timelines. Hybrid solutions, however, hold the fastest 22.85% CAGR forecast, reflecting provider desire to retain sensitive workloads on-premise while off-loading non-PHI analytics to hyperscale services. Vendors now pre-package connectors that let organizations shuttle data across environments without refactoring legacy code, smoothing migration trajectories.
On-premise deployments persist in military hospitals, genomic research institutes, and jurisdictions mandating data localization, though their eHealth market share continues to erode as total cost of ownership rises. The hybrid paradigm also aids multi-cloud strategies, preventing lock-in and aligning compute location with regulatory risk profiles. As cloud regions proliferate and sovereign-cloud offerings mature, the addressable base for fully managed subscriptions expands further, reinforcing a long-run shift toward consumption-based pricing models.
The EHealth Market Report is Segmented by Component (Electronic Health Records, E-Prescribing, Telemedicine, and More), Delivery Mode (Cloud-Based Solutions, and More), Type of Service (Monitoring Service, Diagnosis Service, and Therapeutic Services), End User (Hospitals, Insurance Companies, and More), and Geography (North America, Europe, Asia-Pacific, and More). The Market Forecasts are Provided in Terms of Value (USD).
Geography Analysis
North America produced 42.82% of 2024 revenue, driven by mature reimbursement frameworks, a high clinician-to-patient ratio, and aggressive investment in AI-enabled clinical decision support. The HTI-2 rule and federal AI strategic plan signal long-term regulatory stability, encouraging provider spending and venture capital inflows. Canada advances provincial interoperability initiatives, and cross-border telehealth partnerships allow winter-surge overflow management, while Mexico scales cloud-hosted records to underserved regions. Ongoing cyber-attacks remain a regional restraint, prompting higher security budgets that inflate total cost of ownership for eHealth deployments.
Asia-Pacific delivers the highest 20.61% CAGR, with China's 5G medical pilots, India's insurance-backed digital health stack, and Australia's federally funded interoperability plan as key accelerants. Successful remote robotic surgery across 1,500 km in China validates ultra-low-latency care models and burnishes national AI ambitions bmc. Singapore embeds IoT sensors into public-hospital wards for predictive analytics, while Thailand pursues virtual-care to bridge specialist shortages. Government-led sandbox programs streamline approvals and shorten commercial lead times, sustaining investor confidence in the region's eHealth market.
Europe maintains steady expansion anchored by EUR 810 million earmarked for the European Health Data Space and the risk-based EU AI Act slated for phased compliance by 2027. Germany's 6G Health project positions Europe at the forefront of next-generation connectivity, and the UK's sector-specific AI governance introduces differentiated oversight paths for clinical algorithms. Nordic nations pilot personal-data wallets that give citizens granular consent controls, while Southern European providers upgrade cloud capacity to offset clinician shortages. The regulatory push for trust and safety enhances adoption intent but also raises compliance costs, compelling smaller vendors to seek partnership or acquisition.
- Veradigm
- Athenahealth
- Salesforce Health Cloud
- Oracle
- Microsoft Healthcare
- GE Healthcare
- eClinicalWorks
- Epic Systems
- Optum
- Siemens Healthineers
- Koninklijke Philips
- Teladoc Health
- Amwell (American Well)
- Medtronic
- Mckesson
- Meditech
- Google Cloud Healthcare
- DrChrono Inc.
- NextGen Healthcare
- Kareo
- Dedalus Group
Additional Benefits:
- The market estimate (ME) sheet in Excel format
- 3 months of analyst support
TABLE OF CONTENTS
1 Introduction
- 1.1 Study Assumptions & Market Definition
- 1.2 Scope of the Study
2 Research Methodology
3 Executive Summary
4 Market Landscape
- 4.1 Market Overview
- 4.2 Market Drivers
- 4.2.1 Government Incentives For Digital Health Adoption
- 4.2.2 Growing Prevalence of Chronic Diseases Demanding Remote Monitoring
- 4.2.3 Expansion of High?Speed Connectivity (5G) Enabling Telehealth
- 4.2.4 Integration of Generative-AI Copilots Into EHR Workflows
- 4.2.5 Emergence of Retail & Big-Tech Virtual Clinics
- 4.3 Market Restraints
- 4.3.1 Data Security & Privacy Concerns
- 4.3.2 Interoperability Challenges Among Disparate Systems
- 4.3.3 AI Algorithm Liability & Malpractice Insurance Gaps
- 4.4 Porter's Five Forces
- 4.4.1 Bargaining Power of Suppliers
- 4.4.2 Bargaining Power of Buyers/Consumers
- 4.4.3 Threat of New Entrants
- 4.4.4 Threat of Substitute Products
- 4.4.5 Intensity of Competitive Rivalry
5 Market Size & Growth Forecasts (Value, USD)
- 5.1 By Component
- 5.1.1 Electronic Health Records
- 5.1.2 Telemedicine
- 5.1.3 mHealth Apps
- 5.1.4 Clinical Decision Support
- 5.1.5 e-Prescribing
- 5.1.6 Other Components
- 5.2 By Delivery Mode
- 5.2.1 Cloud-based Solutions
- 5.2.2 On-premise Solutions
- 5.2.3 Hybrid Solutions
- 5.3 By Type of Service
- 5.3.1 Monitoring Services
- 5.3.1.1 Remote Patient Monitoring
- 5.3.1.2 Chronic Disease Management
- 5.3.2 Diagnostic Services
- 5.3.2.1 Tele-radiology
- 5.3.2.2 Tele-pathology
- 5.3.3 Therapeutic Services
- 5.3.3.1 Digital Therapeutics
- 5.3.3.2 Virtual Rehabilitation
- 5.3.1 Monitoring Services
- 5.4 By End User
- 5.4.1 Hospitals & Health Systems
- 5.4.2 Insurance Companies & Payers
- 5.4.3 Patients & Individual Consumers
- 5.4.4 Other End Users
- 5.5 Geography
- 5.5.1 North America
- 5.5.1.1 United States
- 5.5.1.2 Canada
- 5.5.1.3 Mexico
- 5.5.2 Europe
- 5.5.2.1 Germany
- 5.5.2.2 United Kingdom
- 5.5.2.3 France
- 5.5.2.4 Italy
- 5.5.2.5 Spain
- 5.5.2.6 Rest of Europe
- 5.5.3 Asia-Pacific
- 5.5.3.1 China
- 5.5.3.2 Japan
- 5.5.3.3 India
- 5.5.3.4 South Korea
- 5.5.3.5 Australia
- 5.5.3.6 Rest of Asia-Pacific
- 5.5.4 Middle East and Africa
- 5.5.4.1 GCC
- 5.5.4.2 South Africa
- 5.5.4.3 Rest of Middle East and Africa
- 5.5.5 South America
- 5.5.5.1 Brazil
- 5.5.5.2 Argentina
- 5.5.5.3 Rest of South America
- 5.5.1 North America
6 Competitive Landscape
- 6.1 Market Concentration
- 6.2 Market Share Analysis
- 6.3 Company Profiles (includes Global level Overview, Market level overview, Core Segments, Financials as available, Strategic Information, Market Rank/Share for key companies, Products & Services, and Recent Developments)
- 6.3.1 Veradigm LLC
- 6.3.2 athenahealth Inc.
- 6.3.3 Salesforce Health Cloud
- 6.3.4 Oracle Cerner
- 6.3.5 Microsoft Healthcare
- 6.3.6 GE Healthcare
- 6.3.7 eClinicalWorks
- 6.3.8 Epic Systems Corporation
- 6.3.9 Optum Health
- 6.3.10 Siemens Healthineers
- 6.3.11 Koninklijke Philips NV
- 6.3.12 Teladoc Health
- 6.3.13 Amwell (American Well)
- 6.3.14 Medtronic plc
- 6.3.15 McKesson Corporation
- 6.3.16 Meditech
- 6.3.17 Google Cloud Healthcare
- 6.3.18 DrChrono Inc.
- 6.3.19 NextGen Healthcare
- 6.3.20 Kareo
- 6.3.21 Dedalus Group
7 Market Opportunities & Future Outlook
- 7.1 White-space & Unmet-need Assessment




