PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1850048

PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1850048
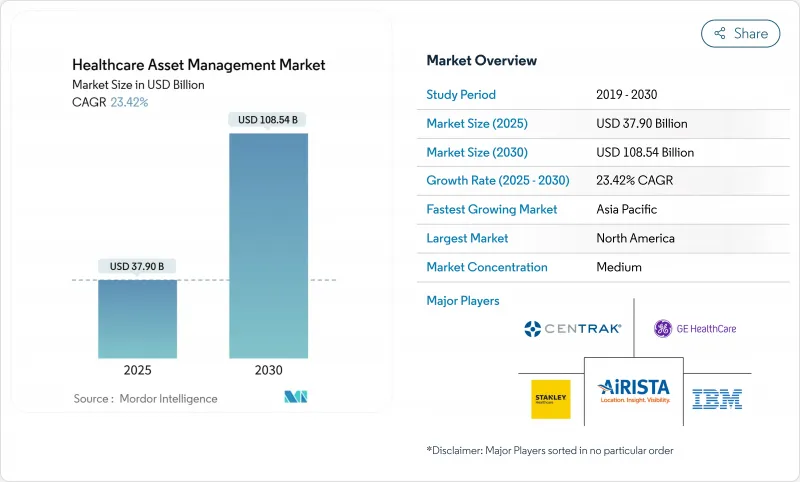
Healthcare Asset Management - Market Share Analysis, Industry Trends & Statistics, Growth Forecasts (2025 - 2030)
The Healthcare Asset Management Market size is estimated at USD 37.90 billion in 2025, and is expected to reach USD 108.54 billion by 2030, at a CAGR of 23.42% during the forecast period (2025-2030).
The growth trajectory reflects how regulatory mandates, workforce shortages, and cybersecurity expectations converge to reposition asset tracking from a cost-containment tool to a strategic pillar of digital health operations. Hospitals are looking beyond bar-code inventory toward connected platforms that streamline compliance with the FDA's 2024 device-security guidance, an obligation that can consume 5% or more of a manufacturer's annual revenue. Demand also ties directly to nursing-staff constraints; shrinking clinical capacity magnifies the value of systems that free caregivers from locating equipment and instead let them focus on patient outcomes. In parallel, predictive analytics embedded in tags move maintenance from reactive to anticipatory, trimming downtime and extending asset life. Taken together, these forces enable a healthcare asset management market environment in which hospitals, pharma plants, and laboratories regard integrated visibility, cybersecurity, and analytics as non-negotiable features rather than optional add-ons.
Global Healthcare Asset Management Market Trends and Insights
Rising demand for RFID to curb drug counterfeiting
Pharmaceutical counterfeiting drains an estimated USD 200 billion from the global economy each year, prompting regulators to impose serialisation and pedigree requirements that make end-to-end visibility indispensable. Under the U.S. Drug Supply Chain Security Act, drug makers, wholesalers, and dispensers must prove product provenance at every hand-off. RFID with cryptographic authentication now underpins most of these deployments because it combines item-level identification with real-time environmental monitoring, a necessity for temperature-sensitive biologics. Semiconductor shortages since 2024 lifted tag prices by up to 20%, yet organisations still invest because non-compliance fines and recall costs far exceed hardware spending. Vendors such as SATO have introduced sterilisation-resistant tags that deliver both authentication and workflow efficiency in one process step. These factors underpin the 26.8% CAGR projected for pharmaceutical and biotech manufacturing customers between 2025 and 2030.
Efficiency pressures from nursing-staff shortages
Nursing vacancy rates above 15% in major urban hospitals leave care teams stretched and force administrators to squeeze every efficiency gain possible from support technology. Studies reveal that nurses spend over one-fifth of each shift searching for missing equipment; RTLS implementations that cut search time by more than 90% therefore provide a direct labour dividend that keeps beds staffed without adding headcount. British facilities have demonstrated time reductions from 60 minutes to 10 minutes per device, translating into heightened patient-safety scores and improved staff retention. Advanced deployments now combine BLE badges, panic buttons, and predictive analytics that stage equipment on units before clinicians request it, easing workflow strain and boosting satisfaction.
Data-privacy and cybersecurity concerns
Average breach costs in healthcare reached USD 9.77 million per incident in 2024, making security risk a material deterrent to rapid roll-outs. The FDA's 2024 draft guidance urges stronger pre-market security testing, compelling buyers to fund encryption, network segmentation, and continuous monitoring before go-live. Many hospitals, therefore, begin with on-premises deployments or air-gapped networks that limit data flow to the cloud, trading some analytics capability for risk reduction. Legacy devices without secure firmware further complicate integrations, extending project timelines and inflating budgets.
Other drivers and restraints analyzed in the detailed report include:
- Patient-safety regulations (UDI, EU-MDR)
- AI-based predictive maintenance embedded in tags
- High upfront RTLS/RFID infrastructure cost
For complete list of drivers and restraints, kindly check the Table Of Contents.
Segment Analysis
RFID accounted for 56.2% of 2024 revenue, underlining decades of protocol maturity and robust supply chains that made the technology the default for drug inventory and surgical kit tracking. The healthcare asset management market size for RFID was USD 21.3 billion in 2024, showing how deeply the modality is entrenched at point-of-care cabinets and central sterile processing. Yet software-defined workflows increasingly require location, not just identity. Real-Time Location Systems leveraging BLE, Wi-Fi, and ultra-wideband are therefore forecast to compound at 28.1% CAGR to 2030, eating into static RFID growth.
A second growth phase emerges as vendors collapse RFID and RTLS into multi-mode tags that pivot between passive ID and real-time telemetry, a design that preserves prior capital investment while enabling richer analytics. Deployments at paediatric-care centres demonstrate this twin-mode value: passive RFID limits shrinkage of high-value drugs, while RTLS ensures infusion pumps circulate where patient acuity is highest. Hardware still dominates spending because tags, gateways, and exciters blanket entire campuses; however, the profit pool is shifting toward platform licences that unite device identity, location, and utilisation into one dashboard. As this convergence proceeds, the healthcare asset management market will likely regard single-mode offerings as a niche.
Hardware captured 62.4% of 2024 sales thanks to ongoing purchases of millions of tags, readers, and ceiling-mounted beacons. Even so, services are pacing ahead with a 25.6% CAGR as hospitals pivot from capital expense toward managed outcomes. Under subscription agreements, vendors guarantee uptime, firmware currency, and regulatory-ready audit logs, freeing IT teams to focus on patient-facing initiatives. The healthcare asset management market size tied to services is forecast to reach USD 32.6 billion by 2030, pointing to a maturation cycle where infrastructure becomes ubiquitous and differentiation shifts to consultative optimisation.
Professional and managed services also address the hardest obstacles-change management, systems integration, and cybersecurity accreditation-that no amount of shelf hardware alone can solve. Service contracts typically bundle remote device health checks, algorithm updates, and compliance documentation generation, costs that spread evenly across multi-year terms and match reimbursement cycles. Hospitals increasingly justify deals by showing that avoided nursing overtime, faster bed turnover, and reduced device rentals offset monthly subscription fees.
Healthcare Asset Management Market is Segmented by Technology (RFID, Real-Time Location Systems, and More), Component (Hardware, Software, and Services), Application (Equipment and Device Tracking, Inventory/Supply-Chain Management, and More), End-User (Hospitals and Clinics, Laboratories and Diagnostic Centers, and More), and Geography. The Market Forecasts are Provided in Terms of Value (USD).
Geography Analysis
North America held 37.8% of 2024 revenue, sustained by the United States' comprehensive serialisation law, a mature EHR backbone, and rising incidents of medical device cyber threats that favour integrated, secure platforms. Canadian provinces are adopting similar policies, while Mexican private-sector hospitals invest in asset tracking to retain medical tourists and satisfy U.S. insurer audits. Government reimbursement models that penalise safety lapses make traceability a board-level metric, further supporting healthcare asset management market adoption across the region.
Asia-Pacific is the fastest-growing area with a 22.5% CAGR expected through 2030. Public-hospital construction programmes in China, India, and Southeast Asia enable greenfield deployments that skip legacy bar-code steps and implement RFID-RTLS convergence from day one. Many of these facilities integrate asset management with national digital-health clouds, allowing real-time drug authentication across regional supply chains. As capital investment aligns with universal health-coverage goals, vendors report multi-year master contracts covering hundreds of new hospitals.
Europe shows steady uptake led by the EU-MDR mandate, EUDAMED database roll-outs, and national sustainability targets that favour lifecycle optimisation. Germany and the United Kingdom drive early deployments, but funding mechanisms in Eastern Europe are catching up as structural funds emphasise digital transformation. Cybersecurity expectations anchored in GDPR elevate demand for on-premises or hybrid clouds with local data residency, nudging platform suppliers to broaden configuration options. With Brexit adding customs complexity for cross-channel medical trade, British providers rely on traceability to avoid port delays and product waste.
- Stanley Healthcare (Stanley Black & Decker)
- CenTrak Inc.
- AiRISTA Flow Inc.
- GE HealthCare Technologies Inc.
- IBM Corporation
- Infor Inc.
- Motorola Solutions Inc.
- Siemens Healthineers AG
- Accenture plc
- Sonitor Technologies AS
- Zebra Technologies Corporation
- Johnson Controls (Tyco International)
- Honeywell International Inc.
- Impinj Inc.
- Alien Technology LLC
- HID Global Corporation
- Ascom Holding AG
- Midmark Corporation (Versus RTLS)
- Trimble Inc. (Atrius)
- Cerner Corporation (Oracle Health)
- TagMaster AB
- Radianse LLC
- Kontakt.io Inc.
- Litum IoT Technologies
- Elpas Ltd. (Securitas)
Additional Benefits:
- The market estimate (ME) sheet in Excel format
- 3 months of analyst support
TABLE OF CONTENTS
1 INTRODUCTION
- 1.1 Study Assumptions and Market Definition
- 1.2 Scope of the Study
2 RESEARCH METHODOLOGY
3 EXECUTIVE SUMMARY
4 MARKET INSIGHTS
- 4.1 Market Overview
- 4.2 Market Drivers
- 4.2.1 Rising demand for RFID to curb drug counterfeiting
- 4.2.2 Efficiency pressures from nursing?staff shortages
- 4.2.3 Patient-safety regulations (e.g., UDI, EU-MDR)
- 4.2.4 AI-based predictive maintenance embedded in tags
- 4.2.5 Pay-for-performance reimbursement tied to asset traceability
- 4.3 Market Restraints
- 4.3.1 Data-privacy and cybersecurity concerns
- 4.3.2 High upfront RTLS/RFID infrastructure cost
- 4.3.3 Radio-interference with critical wireless medical devices
- 4.3.4 Fragmented legacy CMMS slowing integration
- 4.4 Industry Value Chain Analysis
- 4.5 Regulatory Landscape
- 4.6 Technological Outlook
- 4.7 Industry Attractiveness - Porter's Five Forces Analysis
- 4.7.1 Bargaining Power of Suppliers
- 4.7.2 Bargaining Power of Buyers
- 4.7.3 Threat of New Entrants
- 4.7.4 Threat of Substitute Products
- 4.7.5 Intensity of Competitive Rivalry
- 4.8 Impact of Macroeconomic Factors on the Market
5 MARKET SIZE AND GROWTH FORECASTS (VALUES)
- 5.1 By Technology
- 5.1.1 RFID
- 5.1.2 Real-Time Location Systems (RTLS)
- 5.1.3 Bluetooth Low Energy (BLE) and Wi-Fi
- 5.1.4 Infrared and Ultrasound
- 5.2 By Component
- 5.2.1 Hardware (Tags, Readers, Gateways)
- 5.2.2 Software (Analytics, Middleware)
- 5.2.3 Services (Deployment, Managed, Training)
- 5.3 By Application
- 5.3.1 Equipment and Device Tracking
- 5.3.2 Inventory/Supply-Chain Management
- 5.3.3 Patient and Staff Tracking
- 5.3.4 Bed and Capacity Management
- 5.3.5 Environmental and Condition Monitoring
- 5.4 By End-user
- 5.4.1 Hospitals and Clinics
- 5.4.2 Laboratories and Diagnostic Centers
- 5.4.3 Pharmaceutical and Biotech Manufacturing
- 5.4.4 Long-Term Care and Assisted-Living Facilities
- 5.5 By Geography
- 5.5.1 North America
- 5.5.1.1 United States
- 5.5.1.2 Canada
- 5.5.1.3 Mexico
- 5.5.2 South America
- 5.5.2.1 Brazil
- 5.5.2.2 Argentina
- 5.5.2.3 Chile
- 5.5.2.4 Rest of South America
- 5.5.3 Europe
- 5.5.3.1 Germany
- 5.5.3.2 United Kingdom
- 5.5.3.3 France
- 5.5.3.4 Italy
- 5.5.3.5 Spain
- 5.5.3.6 Russia
- 5.5.3.7 Rest of Europe
- 5.5.4 Asia-Pacific
- 5.5.4.1 China
- 5.5.4.2 India
- 5.5.4.3 Japan
- 5.5.4.4 South Korea
- 5.5.4.5 Australia
- 5.5.4.6 Malaysia
- 5.5.4.7 Singapore
- 5.5.4.8 Rest of Asia-Pacific
- 5.5.5 Middle East and Africa
- 5.5.5.1 Middle East
- 5.5.5.1.1 United Arab Emirates
- 5.5.5.1.2 Saudi Arabia
- 5.5.5.1.3 Turkey
- 5.5.5.1.4 Rest of Middle East
- 5.5.5.2 Africa
- 5.5.5.2.1 South Africa
- 5.5.5.2.2 Nigeria
- 5.5.5.2.3 Egypt
- 5.5.5.2.4 Rest of Africa
- 5.5.1 North America
6 COMPETITIVE LANDSCAPE
- 6.1 Market Concentration
- 6.2 Strategic Moves
- 6.3 Market Share Analysis
- 6.4 Company Profiles (includes Global level Overview, Market level overview, Core Segments, Financials as available, Strategic Information, Market Rank/Share for key companies, Products and Services, and Recent Developments)
- 6.4.1 Stanley Healthcare (Stanley Black & Decker)
- 6.4.2 CenTrak Inc.
- 6.4.3 AiRISTA Flow Inc.
- 6.4.4 GE HealthCare Technologies Inc.
- 6.4.5 IBM Corporation
- 6.4.6 Infor Inc.
- 6.4.7 Motorola Solutions Inc.
- 6.4.8 Siemens Healthineers AG
- 6.4.9 Accenture plc
- 6.4.10 Sonitor Technologies AS
- 6.4.11 Zebra Technologies Corporation
- 6.4.12 Johnson Controls (Tyco International)
- 6.4.13 Honeywell International Inc.
- 6.4.14 Impinj Inc.
- 6.4.15 Alien Technology LLC
- 6.4.16 HID Global Corporation
- 6.4.17 Ascom Holding AG
- 6.4.18 Midmark Corporation (Versus RTLS)
- 6.4.19 Trimble Inc. (Atrius)
- 6.4.20 Cerner Corporation (Oracle Health)
- 6.4.21 TagMaster AB
- 6.4.22 Radianse LLC
- 6.4.23 Kontakt.io Inc.
- 6.4.24 Litum IoT Technologies
- 6.4.25 Elpas Ltd. (Securitas)
7 MARKET OPPORTUNITIES AND FUTURE TRENDS
- 7.1 White-Space and Unmet-Need Assessment




