PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1852172

PUBLISHER: Mordor Intelligence | PRODUCT CODE: 1852172
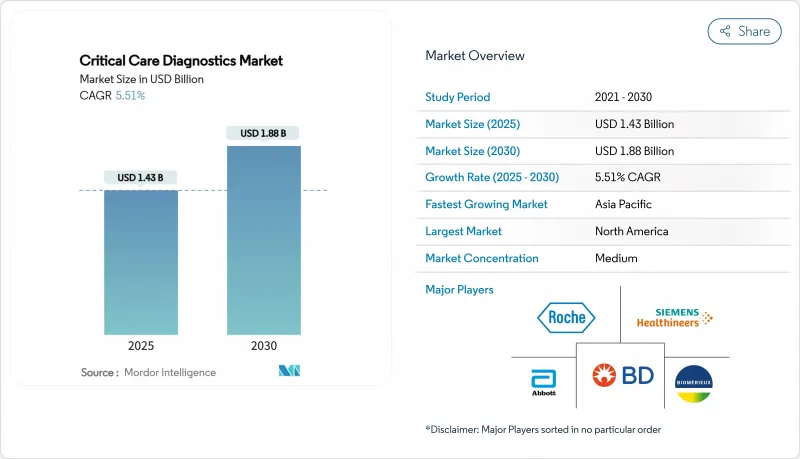
Critical Care Diagnostics - Market Share Analysis, Industry Trends & Statistics, Growth Forecasts (2025 - 2030)
The critical care diagnostics market size is USD 1.43 billion in 2025 and is forecast to reach USD 1.88 billion by 2030, expanding at a 5.51% CAGR.
Intensifying demand for rapid triage inside intensive care units (ICUs), emergency departments and mobile ICUs keeps bedside analyzers at the center of hospital budgets. Growing sepsis, cardiovascular and acute respiratory caseloads reinforce purchasing momentum for instruments that cut result-turnaround from hours to single-digit minutes. Major health-system digitalization programs now seek analyzers that transmit structured data directly to electronic records while AI dashboards translate longitudinal biomarker trends into actionable care pathways. Capital continues to pour in from public infrastructure expansions across Asia-Pacific and from private-equity financing of start-ups with narrowly focused, ultra-fast pathogen and host-response assays, reshaping competitive dynamics and catalyzing device replacement cycles.
Global Critical Care Diagnostics Market Trends and Insights
Growing Burden of Critical Illnesses Requiring Rapid Diagnostics
Sepsis affects more than 1.7 million U.S. adults each year, and mortality jumps when diagnosis is delayed beyond six hours. FDA clearance of the MeMed BV host-response test in 2025 enables clinicians to distinguish bacterial from viral infections in under 20 minutes. Aging populations add multimorbidity to already complex ICU rosters, while emerging markets confront rising trauma and infectious-disease burdens. Predictive algorithms that track high-sensitivity troponin, lactate and procalcitonin can now warn of physiologic decline six to twelve hours before overt symptoms, improving outcomes and reducing resource utilization.
Expansion of Point-of-Care Testing in Acute Care Settings
Hand-held cartridge analyzers eliminate specimen shuttling that previously added 45-90 minutes to turnaround. Devices such as Nova Biomedical's Stat Profile Prime Plus produce 11-parameter panels from 90 µL of capillary blood, preserving sample volume for hemodynamically unstable patients. Emergency rooms that migrated troponin assays from central labs to bedside platforms report 30-40% shorter throughput times. Portable molecular units introduced during the COVID-19 crisis now equip ambulances, allowing thrombolysis or antibiotic therapy to begin even before hospital doors open.
High Capital and Operational Costs of Advanced Diagnostic Platforms
AI-ready blood-gas workstations can cost more than USD 500,000 per unit, while service contracts add roughly 10% annually. Smaller community hospitals hesitate when test volumes cannot guarantee payback. Subscription or outcome-based pricing models have emerged, yet boards often demand multi-year evidence before committing.
Other drivers and restraints analyzed in the detailed report include:
- Integration of Diagnostics into Connected Hospital Ecosystems
- Government and Private Investments in Intensive-Care Infrastructure
- Limited Skilled Workforce in Critical Care Laboratories
For complete list of drivers and restraints, kindly check the Table Of Contents.
Segment Analysis
Hematology tests accounted for 24.45% of the critical care diagnostics market size in 2024, reflecting their role in transfusion decisions, coagulation surveillance and infection monitoring. Automated analyzers now deliver a complete blood count in under 60 seconds and link directly to transfusion-management software. Coagulation sub-panels have expanded with viscoelastic assays that track clot formation in real time, guiding targeted antifibrinolytic therapy during trauma resuscitation.
Routine and special chemistry is set to grow at a 7.65% CAGR, fueled by expanded panels covering high-sensitivity troponins, presepsin and metabolic stress markers that enable early deterioration prediction. Microbiology and molecular pathogen panels advance in tandem with antibiotic stewardship mandates, providing sub-hour susceptibility profiles that curtail broad-spectrum drug use. Flow cytometry retains value for immunosuppressed cohorts in transplant ICUs, while immunoprotein assays broaden with soluble CD14 variants that refine sepsis risk stratification. Collectively, these shifts align with clinician demand for multiplex dashboards that present holistic patient snapshots rather than isolated parameters, positioning integrated platforms at the forefront of procurement decisions.
Point-of-care devices generated 52.56% of 2024 revenue for the critical care diagnostics market and remain essential for collapsing turnaround times at the bedside. Cartridge-based blood-gas analyzers, handheld glucose-ketone meters and compact immunoassay instruments dominate purchase lists because they require minimal maintenance and fit seamlessly into high-acuity workflows.
Yet AI-enabled decision-support systems, projected to expand at a 7.78% CAGR, are reshaping buyer expectations. Middleware hubs equipped with neural networks continuously analyze longitudinal biomarker data to predict adverse events up to 12 hours in advance, triggering protocol-driven interventions. Central-lab analyzers still serve high-throughput needs, but increased decentralization means their future lies in hub-and-spoke architectures that support tiered care settings. Hybrid cloud infrastructures lower entry barriers for community hospitals by offloading computational demands, while cybersecurity enhancements address rising concern over patient-data breaches. Collectively, these developments forecast a technology mix where bedside hardware and cloud intelligence operate in lock-step to bolster clinical outcomes.
The Critical Care Diagnostics Market Report is Segmented by Test Type (Flow Cytometry, Hematology Tests, Microbiology & Infectious Disease Tests, and More), Technology (Central-Lab Analyzers, and More), End User (Intensive Care Units, and More), Sample Type (Whole Blood, and More), and Geography (North America, Europe, Asia-Pacific, Middle East & Africa, South America). The Market Forecasts are Provided in Terms of Value (USD).
Geography Analysis
North America retained 42.45% of 2024 revenue, underpinned by advanced ICU bed density, expansive payer systems and streamlined FDA pathways that allow rapid device clearance. U.S. hospitals continue to integrate AI dashboards to comply with value-based reimbursement, while Canadian provincial tenders emphasize cartridge interoperability across dispersed care settings. Europe follows with robust demand driven by modernization programs and an aging demographic that elevates critical-illness incidence. Germany funds trauma networks that specify viscoelastic coagulation analyzers, and France invests in micro-fluidic molecular platforms to tackle antimicrobial resistance. The United Kingdom's GBP 2.3 billion commitment to community diagnostic centers demonstrates a shift toward decentralized testing.
Asia-Pacific will lead growth at a 6.54% CAGR through 2030 as China and India channel multibillion-dollar budgets into new tertiary hospitals and mobile ICU fleets. Local joint-venture assembly lines reduce import duties, expanding accessibility for mid-tier hospitals. Japan refines AI-assisted sepsis alerts, while South Korea pioneers cloud-connected cardiac troponin networks across regional hospitals. In Southeast Asia, portable PCR and blood-gas analyzers equip rural clinics, bridging health-equity gaps for populations historically distant from laboratory services.
The Middle East and Africa benefit from oil-funded hospital projects in Gulf Cooperation Council states and donor-backed trauma centers in North Africa. South America records stable mid-single-digit gains, with Brazil deploying mobile stroke units fit with CT and blood-gas analyzers to address high cerebrovascular mortality. Together these geographic threads position the critical care diagnostics market for synchronized yet region-specific expansion over the forecast period.
- Abbott Laboratories
- Roche
- Siemens Healthineers
- Danaher (Beckman Coulter & Cepheid)
- bioMerieux
- Sysmex
- Beckton Dickinson
- Thermo Fisher Scientific
- Bayer
- Chembio Diagnostics
- Radiometer Medical
- Instrumentation Laboratory (Werfen)
- Nova Biomedical
- QuidelOrtho
- Werfen Group
- PixCell Medical
- Truvian Health
- EKF Diagnostics
- OptiMedical Systems
- Randox Laboratories
Additional Benefits:
- The market estimate (ME) sheet in Excel format
- 3 months of analyst support
TABLE OF CONTENTS
1 Introduction
- 1.1 Study Assumptions & Market Definition
- 1.2 Scope of the Study
2 Research Methodology
3 Executive Summary
4 Market Landscape
- 4.1 Market Overview
- 4.2 Market Drivers
- 4.2.1 Growing Burden of Critical Illnesses Requiring Rapid Diagnostics
- 4.2.2 Expansion of Point-of-Care Testing in Acute Care Settings
- 4.2.3 Integration of Diagnostics Into Connected Hospital Ecosystems
- 4.2.4 Government and Private Investments in Intensive Care Infrastructure
- 4.2.5 Continuous Technological Innovations Enhancing Test Speed and Accuracy
- 4.2.6 Shift Toward Value-Based Care Emphasizing Early Clinical Decision-Making
- 4.3 Market Restraints
- 4.3.1 High Capital And Operational Costs of Advanced Diagnostic Platforms
- 4.3.2 Limited Skilled Workforce in Critical Care Laboratories
- 4.3.3 Regulatory and Reimbursement Uncertainties for Novel Tests
- 4.3.4 Data Security and Privacy Concerns in Connected Diagnostic Devices
- 4.4 Regulatory Landscape
- 4.5 Porter's Five Forces Analysis
- 4.5.1 Threat Of New Entrants
- 4.5.2 Bargaining Power Of Buyers
- 4.5.3 Bargaining Power Of Suppliers
- 4.5.4 Threat Of Substitutes
- 4.5.5 Competitive Rivalry
5 Market Size & Growth Forecasts (Value, USD)
- 5.1 By Test Type
- 5.1.1 Flow Cytometry
- 5.1.2 Hematology Tests
- 5.1.3 Microbiology & Infectious Disease Tests
- 5.1.4 Coagulation Tests
- 5.1.5 Immunoprotein Assays
- 5.1.6 Routine & Special Chemistry
- 5.1.7 Other Test Types
- 5.2 By Technology
- 5.2.1 Central-Lab Analyzers
- 5.2.2 Point-Of-Care Devices
- 5.2.3 Molecular Diagnostics (PCR/NGS)
- 5.2.4 Immunoassay Platforms
- 5.2.5 Microfluidic & Lab-On-Chip
- 5.2.6 AI-Enabled Decision-Support Systems
- 5.3 By End User
- 5.3.1 Intensive Care Units (ICU)
- 5.3.2 Emergency Rooms (ER)
- 5.3.3 Operating Rooms (OR)
- 5.3.4 Ambulance & Mobile ICUs
- 5.3.5 Other End User
- 5.4 By Sample Type
- 5.4.1 Whole Blood
- 5.4.2 Plasma / Serum
- 5.4.3 Point-Of-Care Capillary
- 5.4.4 Respiratory Secretions
- 5.4.5 Other Sample Types
- 5.5 Geography
- 5.5.1 North America
- 5.5.1.1 United States
- 5.5.1.2 Canada
- 5.5.1.3 Mexico
- 5.5.2 Europe
- 5.5.2.1 Germany
- 5.5.2.2 United Kingdom
- 5.5.2.3 France
- 5.5.2.4 Italy
- 5.5.2.5 Spain
- 5.5.2.6 Rest of Europe
- 5.5.3 Asia-Pacific
- 5.5.3.1 China
- 5.5.3.2 Japan
- 5.5.3.3 India
- 5.5.3.4 Australia
- 5.5.3.5 South Korea
- 5.5.3.6 Rest of Asia-Pacific
- 5.5.4 Middle East & Africa
- 5.5.4.1 GCC
- 5.5.4.2 South Africa
- 5.5.4.3 Rest of Middle East & Africa
- 5.5.5 South America
- 5.5.5.1 Brazil
- 5.5.5.2 Argentina
- 5.5.5.3 Rest of South America
- 5.5.1 North America
6 Competitive Landscape
- 6.1 Market Concentration
- 6.2 Market Share Analysis
- 6.3 Company Profiles (includes Global level Overview, Market level overview, Core Business Segments, Financials, Headcount, Key Information, Market Rank, Market Share, Products and Services, and analysis of Recent Developments)
- 6.3.1 Abbott
- 6.3.2 F. Hoffmann-La Roche
- 6.3.3 Siemens Healthineers
- 6.3.4 Danaher (Beckman Coulter & Cepheid)
- 6.3.5 bioMerieux
- 6.3.6 Sysmex Corporation
- 6.3.7 Becton, Dickinson & Company
- 6.3.8 Thermo Fisher Scientific
- 6.3.9 Bayer AG
- 6.3.10 Chembio Diagnostics
- 6.3.11 Radiometer Medical
- 6.3.12 Instrumentation Laboratory (Werfen)
- 6.3.13 Nova Biomedical
- 6.3.14 QuidelOrtho
- 6.3.15 Werfen Group
- 6.3.16 PixCell Medical
- 6.3.17 Truvian Health
- 6.3.18 EKF Diagnostics
- 6.3.19 OptiMedical Systems
- 6.3.20 Randox Laboratories
7 Market Opportunities & Future Outlook
- 7.1 White-Space & Unmet-Need Assessment




